Understanding Cervical Myotomes: A Guide To Nerve Function
Can a seemingly simple neck ache hold the key to understanding complex neurological pathways? The intricate relationship between our cervical nerves, the muscles they control, and the areas of skin they serve, unveils a fascinating landscape of human anatomy and potential dysfunction.
The human body, a marvel of interconnected systems, often reveals its secrets through the smallest of clues. When a cervical nerve, those crucial messengers of the neck, becomes irritated or compressed, it sets off a cascade of events. These events manifest as pain or functional impairments directly related to its dermatome (the area of skin it supplies with sensation) and myotome (the group of muscles it controls for movement). This intimate connection is not just a matter of anatomy; it's a clinical tool, a diagnostic guide that helps unravel the complexities of neurological disorders.
Understanding the cervical spine's intricate network of nerves, muscles, and dermatomes is crucial for healthcare professionals. Clinicians frequently encounter patients battling neck pain, a condition with a significant impact on both personal well-being and economic costs [1, 2]. The ability to accurately assess the cervical spine, therefore, is paramount. This comprehensive article delves into the world of myotomes and dermatomes, exploring their clinical significance, assessment techniques, and implications for diagnosis and treatment, particularly in the context of cervical radiculopathy.
Let's delve into the information about the condition, which involves nerve compression in the cervical spine, its implications, and how to assess and address it.
| Aspect | Details |
|---|---|
| Definition of Cervical Radiculopathy | A disorder stemming from compression, traction, irritation, or herniation affecting a spinal nerve root within the cervical spine. |
| Common Symptoms | Neck pain, radiating arm pain, numbness, sensory deficits, and/or motor dysfunction in the neck and upper extremities. |
| Anatomical Basis | Involves specific dermatomes (areas of skin innervated by a single spinal nerve) and myotomes (groups of muscles controlled by a single spinal nerve root). |
| Clinical Presentation | Typically presents with a predictable pattern of dermatomal and myotomal involvement, reflecting the affected cervical root. |
| Diagnostic Accuracy | Unfortunately, many neurologic indicators used in diagnosis have limited accuracy in real-world scenarios [5, 6]. |
| Assessment Methods | Includes evaluation of the upper limbs using tests like the upper limb tension test, Spurling's test, distraction test, and Valsalva test. Medical Research Council (MRC) scores and EMG findings are often reviewed. |
| Rehabilitation Strategies | Involves specific movement pattern, exercises, and traction. |
| Surgical Interventions | When non-surgical methods fail, surgical approaches are considered. These methods aim to alleviate nerve compression, such as discectomy or laminectomy. |
| Resources | Mayo Clinic: Cervical radiculopathy |
The story of our understanding of cervical dermatomes and myotomes begins with the research of German neurologist and neurosurgeon, Ofid Foerster. In the 1930s, Foerster published two seminal works that laid the groundwork for mapping these crucial neurological areas. These early studies, while providing valuable insights, also highlight the complexities of the human nervous system.
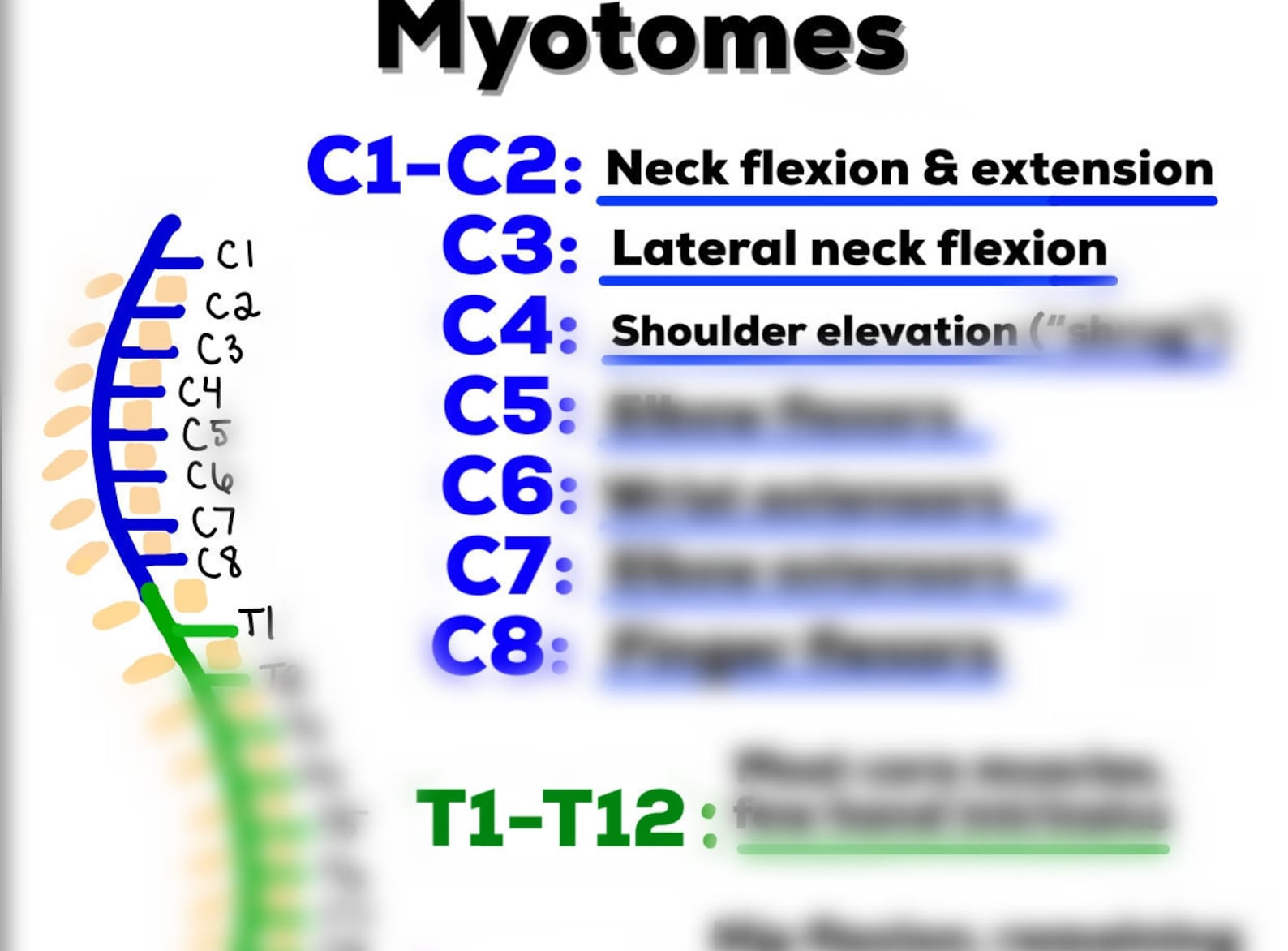
A myotome, as defined by medical professionals, represents a group of muscles innervated by a single spinal nerve root. Conversely, a dermatome is the area of skin that a specific spinal nerve supplies sensation to. They function as a road map for understanding where problems are occurring in the nervous system and at what levels. Clinically, their application is immense, as they help determine if damage has impacted the spinal cord, and pinpoint the exact level of the injury. It is essential that clinicians can confidently perform a thorough assessment of the cervical spine, considering both dermatomal and myotomal patterns.
Cervical and thoracic myotomes are primarily linked to the upper limbs and neck. Specific nerve roots can be tested through isolated muscle group assessment; for example, the triceps muscle corresponds well to the C7 nerve root. However, some nerve roots, like C6, are not easily isolated and supply multiple muscle groups.
The concept of myotomes is vital in diagnosing disorders impacting the spinal and peripheral nerves. Myotomes, are groups of muscles innervated by a single spinal nerve root. This provides a unique insight into understanding neurological deficits after nerve injuries. The myotome of a muscle is the basis for diagnosing spinal and peripheral nerve disorders.
Researchers have methodically charted the connection between specific muscle movements and their associated myotomes. These myotomes cover cervical (C), thoracic (T), lumbar (L), and sacral (S) regions, and while these are the major spinal levels associated with each movement, many movements are influenced by more than one level.
The C3 spinal nerve dermatome typically includes the skin over parts of the upper neck. The corresponding C3 myotome often includes certain neck muscles that assist in bending the neck forward. When assessing the upper limb for cervical radiculopathy, it is important to be aware of the muscles, tests, and sensitivity/specificity associated with each myotome level.
The assessment of myotomes involves a careful examination of muscle strength and function. A healthcare professional will test specific muscle groups, noting any weakness or pain that may indicate nerve root involvement. For example, the C5 myotome is often assessed by evaluating shoulder abduction (raising the arm to the side), while the C7 myotome is tested through elbow extension (straightening the arm).
To aid in memorization and clinical application, a mnemonic device utilizes rhyming patterns to recall the upper myotomes. For example, C2 is associated with "look at your shoe" for cervical flexion, C3 with "a fallen tree" for lateral flexion, C4 with "I'm not sure" for shoulder elevation, C5 with "arms out wide" for shoulder abduction, C6 with "smell your wrist" for wrist extension and elbow flexion, and C7 with "no zombies in heaven" for elbow extension and wrist flexion.
Cervical radiculopathy, a painful condition caused by nerve root compression, is defined as a disorder (compression, traction, irritation, herniated disk) affecting a spinal nerve root in the cervical spine. It is a common cause of pain in the upper extremity. Cervical radiculopathy typically produces neck and radiating arm pain, numbness, sensory deficits, or motor dysfunction in the neck and upper extremities.
Studies have shown that variations exist in both cervical myotomes and dermatomes. Although dermatomes often show little overlap, myotomes typically have more extensive muscle coverage due to shared spinal nerve roots. Furthermore, it's worth noting that while dermatomes are supplied by a single spinal nerve root, the cervical myotomes may include muscles innervated by multiple spinal nerve roots. This is why, the C6 nerve root, for example, is not easily isolated.
A thorough understanding of myotomes, dermatomes, and the clinical tests associated with them is essential for accurately diagnosing and managing conditions like cervical radiculopathy. It allows clinicians to pinpoint the source of the problem, design targeted treatment plans, and monitor the patient's progress effectively.
The assessment includes tests such as the upper limb tension test, Spurling's test, distraction test, and the Valsalva test. A study on the subject presented methods of medical research council (MRC) scores and EMG findings.
By examining myotomes, clinicians can diagnose issues like spinal cord damage and pinpoint where damage has occurred. Further, a study of cervical radiculopathy, found that it typically presents with a reproducible pattern of dermatome and myotome involvement.
As medicine and science continue to advance, the study of myotomes and dermatomes remains essential.