Staph Infection Guide: Symptoms, Causes & Treatment - Mayo Clinic
Could a seemingly harmless bacterium be lurking, ready to unleash a cascade of health crises? Staphylococcus aureus, a common bacterium, can be the culprit behind a range of infections, from minor skin irritations to life-threatening conditions like toxic shock syndrome.
Staph infections, as they are commonly known, are a widespread concern, affecting people of all ages and backgrounds. While many individuals carry staph bacteria without experiencing any adverse effects, the potential for these bacteria to invade the body and cause illness is ever-present. Understanding the various forms of staph infections, their causes, symptoms, and treatments is crucial for prevention and effective management.
Staphylococcus aureus, the primary culprit behind these infections, resides on our skin and in our noses, often without causing harm. However, when the bacteria find their way into the body, usually through a break in the skin, the potential for infection arises. This can manifest in several ways, ranging from localized skin issues to more severe systemic illnesses. The spectrum of staph infections is broad, reflecting the adaptability of the bacteria and its capacity to affect different parts of the body.
The severity of a staph infection depends on a variety of factors, including the specific type of infection, the overall health of the individual, and the presence of antibiotic resistance. One particularly concerning form of staph is methicillin-resistant Staphylococcus aureus (MRSA), a strain resistant to many commonly used antibiotics. MRSA infections can be more difficult to treat and pose a significant challenge in healthcare settings.
Let's delve deeper into the intricacies of staph infections, exploring their diverse manifestations and the importance of recognizing and addressing them promptly.
Understanding Staph Infections: A Comprehensive Overview
Staph infections are caused by bacteria belonging to the Staphylococcus genus, with Staphylococcus aureus being the most common culprit. These bacteria are remarkably resilient, capable of surviving on various surfaces and in diverse environments. They can be found on the skin, in the nose, and on medical equipment, making them a constant presence in our surroundings.
The bacteria typically gain entry into the body through a break in the skin, such as a cut, abrasion, or surgical incision. Once inside, they can multiply and release toxins, leading to a range of infections. The type of infection that develops depends on where the bacteria take hold and how the body responds.
Many healthy individuals carry staph bacteria without experiencing any symptoms. This is known as colonization. The bacteria are present but not causing any harm. However, if the bacteria enter the body through a wound or other breach in the skin, an infection can develop.
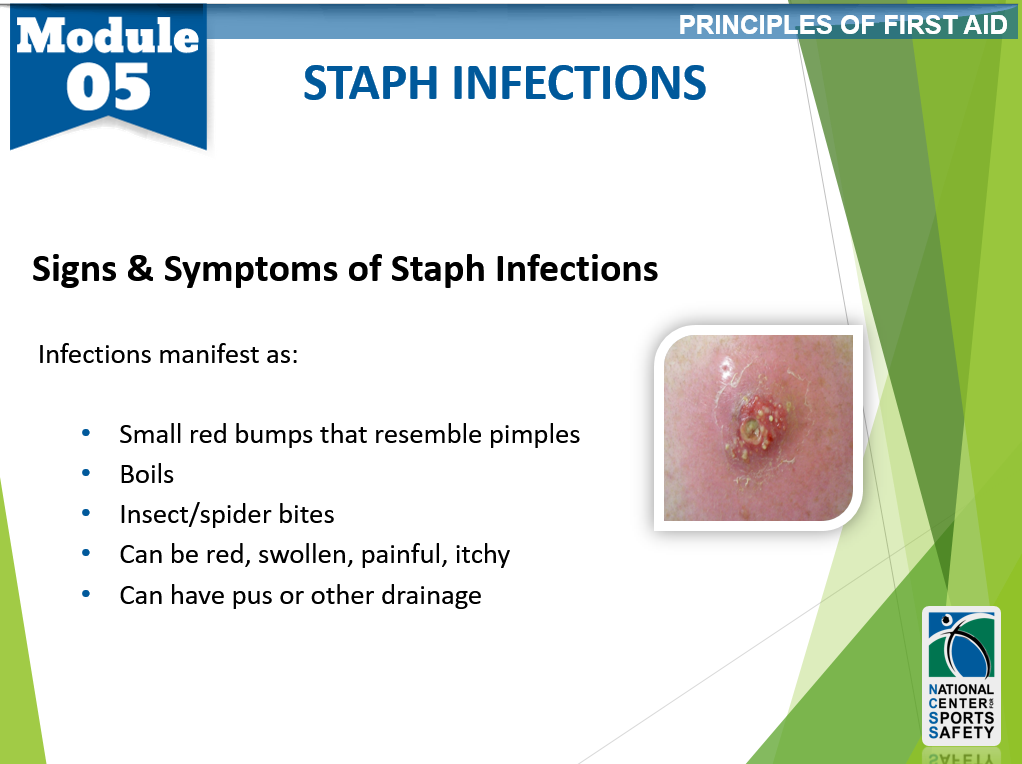
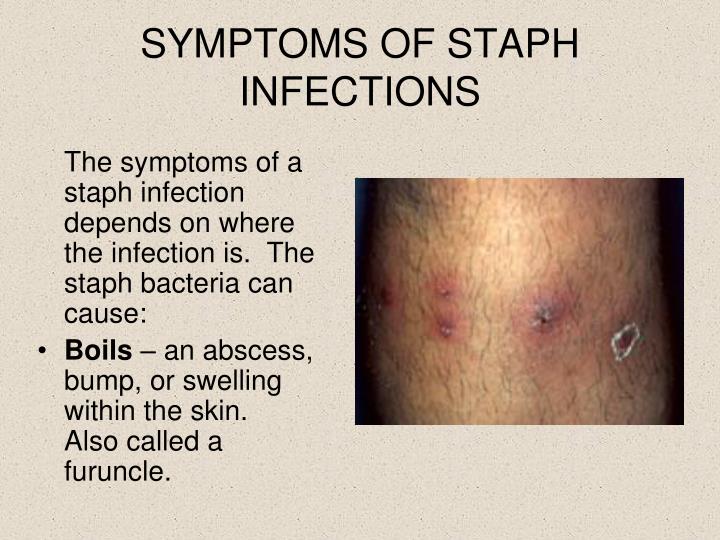
Staph infections can manifest in many different forms. Some are relatively minor, while others can be life-threatening. The signs and symptoms of a staph infection will vary depending on the type of infection. Skin infections are a common presentation.
Types of Staph Infections and Their Manifestations
Staph infections come in many forms, each with unique characteristics and symptoms. The following are some of the most common types of staph infections:
- Skin Infections: These are the most frequently encountered type of staph infection. They can range from mild to severe, and include:
- Folliculitis: Inflammation of hair follicles, often presenting as small, red bumps or pimples.
- Impetigo: A highly contagious skin infection characterized by red sores that form a crust.
- Cellulitis: A deeper skin infection that causes redness, swelling, pain, and warmth.
- Boils and Carbuncles: Pus-filled lumps that can be quite painful.
- Bacteremia: This is a bloodstream infection, also known as blood poisoning. It occurs when staph bacteria enter the bloodstream. Bacteremia can be very serious and requires immediate medical attention. Symptoms may include fever, chills, rapid heartbeat, and confusion.
- Pneumonia: A lung infection caused by staph bacteria. This can lead to severe respiratory symptoms, including cough, chest pain, and difficulty breathing.
- Osteomyelitis: An infection of the bone, often leading to pain, swelling, and fever.
- Endocarditis: An infection of the heart's inner lining and valves. This is a life-threatening condition that requires prompt treatment.
- Toxic Shock Syndrome (TSS): A rare but life-threatening illness caused by toxins produced by certain strains of staph bacteria. Symptoms include high fever, rash, peeling skin, and organ failure.
- Food Poisoning: Staph bacteria can produce toxins that contaminate food, leading to food poisoning. Symptoms include nausea, vomiting, diarrhea, and abdominal cramps.
Recognizing the Signs and Symptoms
The symptoms of a staph infection can vary greatly depending on the type of infection and the area affected. Being able to recognize these signs is essential for seeking prompt medical care. Heres a breakdown of common symptoms:
- Skin Infections:
- Redness, swelling, and pain at the site of infection
- Pus-filled blisters or sores
- Boils or carbuncles (painful, pus-filled lumps)
- Warmth and tenderness to the touch
- Bacteremia (Blood Infection):
- Fever and chills
- Rapid heartbeat
- Confusion or disorientation
- Pneumonia:
- Cough, which may produce phlegm
- Chest pain
- Difficulty breathing
- Osteomyelitis (Bone Infection):
- Pain in the affected bone
- Swelling, warmth, and tenderness around the bone
- Fever
- Endocarditis (Heart Infection):
- Fever
- Fatigue
- Heart murmur
- Toxic Shock Syndrome (TSS):
- High fever
- Rash that looks like a sunburn
- Peeling skin (especially on the palms and soles)
- Vomiting and diarrhea
- Organ failure
- Food Poisoning:
- Nausea and vomiting
- Diarrhea
- Abdominal cramps
Causes and Risk Factors
Staph infections occur when staph bacteria enter the body, usually through a break in the skin. Several factors can increase the risk of developing a staph infection:
- Skin Injury: Cuts, scrapes, burns, insect bites, or surgical incisions provide entry points for staph bacteria.
- Weakened Immune System: People with weakened immune systems, such as those with HIV/AIDS, diabetes, or undergoing chemotherapy, are more susceptible to infection.
- Hospitalization: Hospitalized patients are at increased risk due to exposure to staph bacteria and invasive medical procedures.
- Sharing Personal Items: Sharing towels, razors, or other personal items can spread staph bacteria.
- Contact Sports: Athletes, particularly those in contact sports, are at higher risk due to skin-to-skin contact and the potential for abrasions.
- Crowded Living Conditions: Living in close quarters can increase the risk of staph transmission.
- Use of Invasive Medical Devices: Catheters, intravenous lines, and other medical devices can provide a pathway for staph bacteria to enter the body.
Diagnosis and Treatment
Diagnosing a staph infection typically involves a combination of physical examination and laboratory tests. The doctor will examine the affected area and inquire about symptoms. Laboratory tests may include:
- Culture: A sample of fluid or tissue from the infected area is taken and cultured to identify the specific type of staph bacteria.
- Blood Tests: Blood tests may be performed to detect signs of infection and to check for bacteremia.
- Imaging Tests: X-rays, CT scans, or MRI scans may be used to assess the extent of an infection, especially in cases of bone or deep tissue infections.
Treatment for staph infections depends on the severity and location of the infection, as well as the antibiotic resistance of the bacteria. Common treatment options include:
- Antibiotics: Antibiotics are the mainstay of treatment for most staph infections. The specific antibiotic used will depend on the type of staph bacteria and its antibiotic resistance profile. In the case of MRSA, specific antibiotics are required.
- Drainage of Abscesses: For skin infections with boils or abscesses, the doctor may need to drain the pus to promote healing.
- Wound Care: Proper wound care, including cleaning and dressing the wound, is essential to prevent further spread of the infection.
- Intravenous Antibiotics: Severe infections, such as bacteremia, pneumonia, or endocarditis, often require intravenous antibiotics administered in a hospital setting.
- Surgery: In some cases, surgery may be necessary to remove infected tissue or to repair damage caused by the infection.
Preventing Staph Infections
While staph bacteria are ubiquitous, there are steps individuals can take to reduce the risk of infection:
- Practice Good Hygiene: Wash hands frequently with soap and water, especially after touching potentially contaminated surfaces.
- Keep Wounds Clean: Clean and cover any cuts, scrapes, or abrasions promptly. Change the dressing regularly.
- Avoid Sharing Personal Items: Do not share towels, razors, or other personal items.
- Maintain Skin Health: Keep skin moisturized to prevent cracks and dryness.
- Avoid Contact with Infected Individuals: Limit contact with people who have staph infections.
- Proper Food Handling: Ensure food is cooked thoroughly, and practice safe food handling techniques.
- Seek Prompt Medical Attention: If you suspect you have a staph infection, consult a doctor immediately. Early diagnosis and treatment can prevent complications.
- Be Cautious in High-Risk Settings: Take extra precautions in hospitals, gyms, and other settings where staph infections are more common.
MRSA: A Special Consideration
Methicillin-resistant Staphylococcus aureus (MRSA) is a particularly concerning strain of staph bacteria that has developed resistance to many commonly used antibiotics. MRSA infections can be more difficult to treat and can lead to serious complications. MRSA is often associated with healthcare settings but can also occur in the community.
MRSA infections are often more aggressive and can quickly spread. If you suspect a MRSA infection, its critical to seek medical attention immediately. Treatment for MRSA usually involves specific antibiotics that are effective against resistant strains.
The Broader Impact of Staph Infections
The consequences of staph infections extend beyond the individual affected. Staph infections, especially MRSA, contribute to the rising problem of antibiotic resistance, a major public health threat. The overuse and misuse of antibiotics have fueled the evolution of resistant bacteria, making infections harder to treat and increasing the risk of treatment failure. This can lead to prolonged hospital stays, higher healthcare costs, and, in some cases, death.
Furthermore, staph infections can place a significant burden on healthcare systems. The need for specialized treatment, isolation precautions, and infection control measures to prevent the spread of staph bacteria increases the complexity and cost of care. Infections acquired in hospitals can also lead to staff shortages and disrupt essential services.
Living with Staph Infections
For those who experience recurrent staph infections or complications, the condition can significantly impact quality of life. Skin infections can cause physical discomfort, embarrassment, and social isolation. Chronic or severe infections can lead to limitations in daily activities and the need for ongoing medical care.
Individuals with chronic conditions, such as diabetes or immune deficiencies, may be more susceptible to staph infections. These infections can exacerbate existing health problems, leading to a cycle of illness and reduced well-being. Psychological distress, including anxiety and depression, may also arise due to the uncertainty and challenges associated with recurrent infections.
The Role of Public Health and Prevention
Public health initiatives play a crucial role in controlling and preventing staph infections. Surveillance programs track the prevalence of staph infections, identify outbreaks, and monitor antibiotic resistance patterns. These efforts help inform targeted prevention strategies and guide antibiotic stewardship programs.
Public health education is essential to increase awareness about staph infections, promote preventive measures, and dispel misconceptions. Educating the public about proper hygiene, wound care, and the importance of seeking prompt medical attention is essential. Additionally, promoting responsible antibiotic use is vital to combat antibiotic resistance.
Research and Future Directions
Ongoing research is actively exploring new avenues for preventing and treating staph infections. Scientists are investigating novel antibiotics, developing vaccines, and examining innovative approaches to infection control. These efforts aim to enhance the effectiveness of treatment, reduce the spread of infection, and mitigate the impact of antibiotic resistance.
Research is also focused on identifying risk factors for staph infections and developing targeted prevention strategies. Studying the behavior and evolution of staph bacteria can help create more effective interventions. Moreover, research into the host-pathogen interaction may lead to a better understanding of individual susceptibility to infection.
Conclusion: Taking Action Against Staph Infections
Staph infections pose a significant public health challenge, requiring a multi-faceted approach to prevent, diagnose, and treat them effectively. Recognizing the diverse manifestations of staph infections, understanding the risk factors, and practicing preventive measures are essential for protecting individual and community health. Early detection, appropriate medical care, and responsible antibiotic use are critical to minimize the impact of these infections.
As scientific knowledge advances, new opportunities to prevent and combat staph infections will emerge. By working collaboratively, we can reduce the burden of these infections and safeguard the health and well-being of individuals and communities.
Table: Staph Infection - Key Facts
| Aspect | Details |
|---|---|
| What is it? | A bacterial infection caused by Staphylococcus aureus. |
| Common Types | Skin infections (folliculitis, impetigo, cellulitis, boils), bacteremia, pneumonia, osteomyelitis, endocarditis, toxic shock syndrome, food poisoning. |
| Symptoms | Vary widely depending on infection type: Redness, swelling, pain, pus-filled sores, fever, chills, difficulty breathing, etc. |
| Causes | Entry of staph bacteria into the body, often through a break in the skin. |
| Risk Factors | Skin injuries, weakened immune system, hospitalization, sharing personal items, contact sports, crowded living conditions, invasive medical devices. |
| Diagnosis | Physical examination, culture, blood tests, imaging tests. |
| Treatment | Antibiotics, drainage of abscesses, wound care, intravenous antibiotics, surgery (in some cases). |
| Prevention | Good hygiene, cleaning wounds, avoiding sharing personal items, maintaining skin health, avoiding contact with infected individuals, proper food handling, prompt medical attention, caution in high-risk settings. |
| MRSA | Methicillin-resistant Staphylococcus aureus: A dangerous, antibiotic-resistant strain. |
| Reference | Centers for Disease Control and Prevention (CDC) - MRSA |
:max_bytes(150000):strip_icc()/staph-infections-3156887-FINAL2-48c3a7caea8f429a94f7d074e66d5842.png)