Understanding Meningitis: Types, Symptoms, Prevention & More
Is a seemingly innocuous headache a cause for alarm? Meningitis, an inflammation of the protective membranes surrounding the brain and spinal cord, can manifest in a myriad of ways, and recognizing the symptoms is the first crucial step in safeguarding your health.
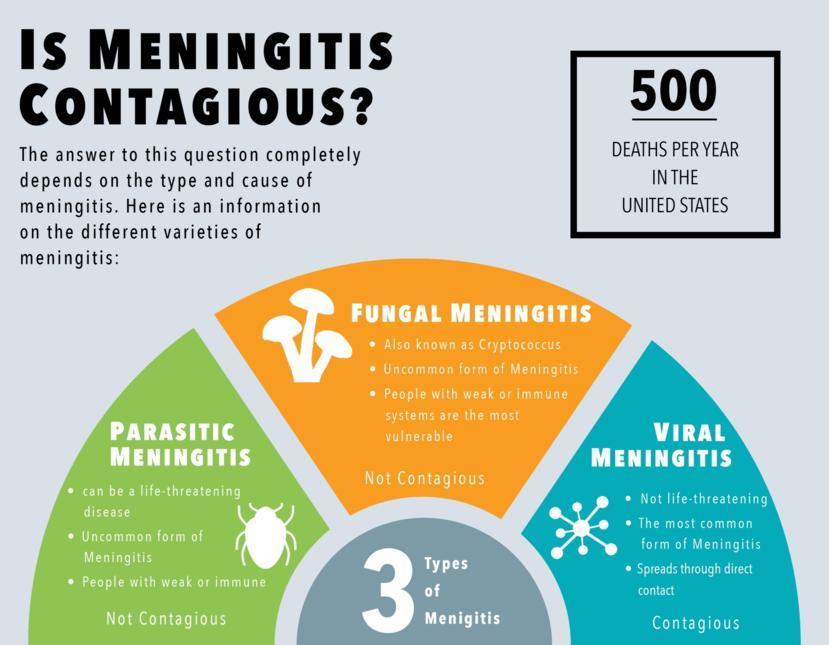
Meningitis, in essence, is a swelling of the meninges, the membranes that meticulously envelope the brain and spinal cord. This inflammation can stem from a variety of sources viral, bacterial, fungal, parasitic, or even injury-induced. Understanding the underlying cause is paramount, as it dictates the severity of the illness, the mode of transmission, and the most effective course of treatment. While some forms of meningitis are contagious, others are not, further underscoring the importance of accurate diagnosis and prompt intervention.
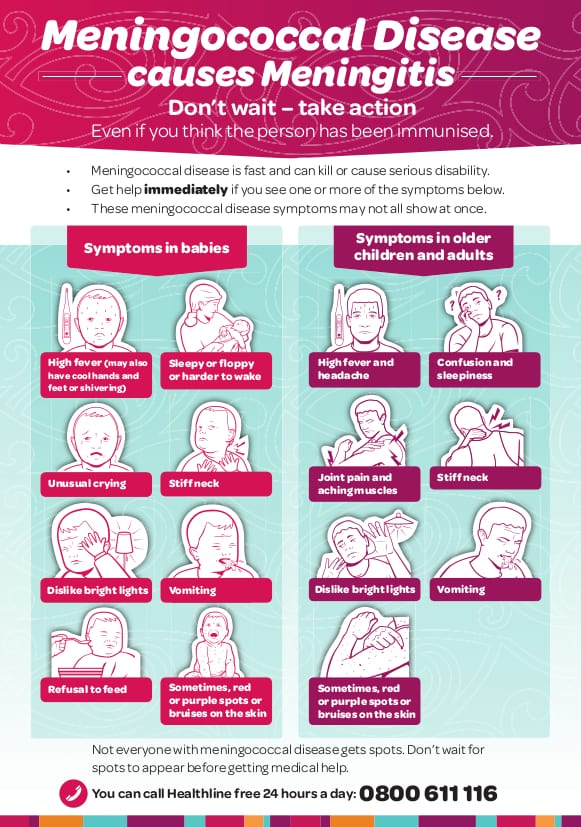
This intricate disease presents a multifaceted challenge. Symptoms range from the classic headache, stiff neck, and fever to more severe presentations like nausea, vomiting, and mental changes. The contagiousness of the disease can vary widely, contingent on the causal agent. For instance, viral meningitis is often less severe than bacterial meningitis, although all suspected cases warrant immediate medical attention. Bacterial meningitis, on the other hand, can progress rapidly and become life-threatening within hours. The disease can affect anyone, but it is most common in babies, young children, teenagers and young adults.
Considering the various potential causes and the complexity of the disease, here is an overview of the types, symptoms, diagnosis, treatment and prevention of meningitis:
| Type of Meningitis | Causative Agent | Transmission | Symptoms | Treatment | Prevention |
|---|---|---|---|---|---|
| Viral Meningitis | Viruses (e.g., enteroviruses, herpes simplex virus) | Direct contact with respiratory secretions (e.g., saliva, nasal mucus) | Headache, stiff neck, fever, nausea, vomiting, sensitivity to light, sleepiness, mental changes | Rest, fluids, pain relievers. Antiviral medications for certain viruses | Good hygiene practices (frequent handwashing), avoid close contact with infected individuals, vaccination for some viruses |
| Bacterial Meningitis | Bacteria (e.g., Neisseria meningitidis, Streptococcus pneumoniae, Haemophilus influenzae) | Respiratory droplets, close contact with infected individuals | Sudden onset of high fever, severe headache, stiff neck, confusion, nausea, vomiting, seizures, petechial rash | Intravenous antibiotics, corticosteroids, supportive care | Vaccination (e.g., meningococcal vaccine, pneumococcal vaccine, Hib vaccine), antibiotics for close contacts |
| Fungal Meningitis | Fungi (e.g., Cryptococcus, Histoplasma) | Inhalation of fungal spores (usually from the environment) | Fever, headache, stiff neck, nausea, vomiting, sensitivity to light, mental changes, confusion | Antifungal medications (e.g., amphotericin B, fluconazole) | Avoidance of exposure to fungal spores (e.g., in soil or bird droppings) - is rare and depends on the environmental conditions |
| Parasitic Meningitis | Parasites (e.g., Naegleria fowleri, Angiostrongylus cantonensis) | Exposure to contaminated water or food | Fever, headache, stiff neck, nausea, vomiting, confusion, seizures | Antiparasitic medications, supportive care | Avoidance of contaminated water, food, and exposure to infected hosts |
| Non-Infectious Meningitis (e.g., Chemical) | Chemicals, medications, or other non-infectious causes | Exposure to chemicals or other irritants | Headache, stiff neck, fever, nausea, vomiting | Treatment is directed at the underlying cause. | Avoidance of exposure to causative agent |
Meningitis is not always highly contagious. However, both viral meningitis and bacterial meningitis can spread through direct contact with nose and throat secretions. It is crucial to note that healthy individuals, who show no apparent signs of illness, can still carry the bacteria in their nose or throat and inadvertently transmit them to others.
Meningococcal meningitis, specifically, is caused by the bacteria Neisseria meningitidis. There are different strains of this bacteria, with serogroups B, C, and Y being the most prevalent in the United States. The disease manifests through inflammation of the meninges and is characterized by a sudden onset of high fever, neck stiffness, confusion, nausea, vomiting, lethargy, and often a petechial or purpuric rash. Early diagnosis and prompt treatment with antibiotics are critical for survival and minimizing the risk of long-term complications.
The diagnostic process for meningitis typically involves a physical examination to assess the symptoms, followed by a lumbar puncture (spinal tap) to analyze cerebrospinal fluid (CSF). This analysis can help identify the causative agent and guide treatment decisions. Blood tests may also be conducted to aid in diagnosis.
The treatment approach varies depending on the type of meningitis. Bacterial meningitis necessitates immediate treatment with intravenous antibiotics, and often corticosteroids to reduce inflammation. Viral meningitis may require supportive care such as rest, fluids, and pain relievers, with antiviral medications reserved for specific viral infections. Fungal and parasitic meningitis require targeted antifungal and antiparasitic drugs, respectively.
Prevention strategies include vaccination against common bacterial strains (such as the meningococcal vaccine) and practicing good hygiene, which involves frequent handwashing and avoiding close contact with individuals who are sick. For those exposed to someone with bacterial meningitis, post-exposure prophylaxis, such as antibiotics, may be recommended to prevent infection.
While the viruses that cause viral meningitis can spread easily, the illness itself is not always easily transmissible. However, the Centers for Disease Control and Prevention (CDC) provides comprehensive guidelines regarding who needs post-exposure prophylaxis, how to diagnose and treat patients, and the vaccines recommended for healthcare personnel.
Meningitis is an infection of the membranes that surround the brain and spinal cord, known as the meninges. This can be caused by various factors, including viruses, bacteria, fungi, or parasites. Prompt medical attention is necessary. If you are exposed to a person with viral meningitis, there is a chance you could become infected with the virus causing the illness. Meningitis refers to swelling and inflammation of the meninges, which constitute a protective layer over the brain. Meningitis can result from a contagious infection, caused by a viral, bacterial, or fungal origin. This underscores the significance of understanding the source and implementing appropriate preventative measures and timely treatment strategies.
The information provided in this article is intended for general knowledge and informational purposes only, and does not constitute medical advice. It is essential to consult with a qualified healthcare professional for any health concerns or before making any decisions related to your health or treatment.